|
| Figure 1 |
 |
| Figure 2 |
 |
| Figure 3 |
 |
| Figure 4 |
 |
| Figure5 |
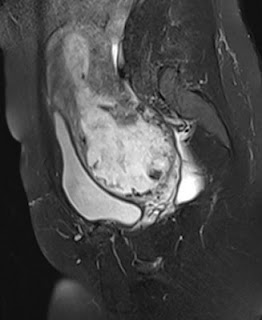
Figures 1 to 5 ( T1, STIR coronal images) show cartilaginous
intra-articular masses or overgrowth along with ossification arising from the
medial aspect of left distal femoral, proximal tibial and distal tibial
epiphyses with resultant deformity of the knee and ankle joints and limb length
discrepancy. This fits into the classic form of Trevor Fairbank disease/
Dysplasia sepiphysealis hemilelica.
BACKGROUND AND HISTORY: Dysplasia epiphysealis hemimelica is a rare development disorder of epiphyses in children.
Mouchet and Berlot described it in 1926 in tarsal bones calling it "tarsomegalie".
In 1950, Treor described 10 cases naming it as "tarsoepiphyseal aclasis"
In 1956, Fairbank described 14 cases and coined the term "dysplasia epiphysealis hemimelica".
The disease is thought to be an osteochondroma of the joint.
It is mostly described in epiphyses and also occurs in seasmoid bones like the patella.
It is most commonly described in lower limb, mainly involving the knee and ankle.
It is hemimelic affecting the medial or lateral aspect of ossification centre, being twice as common in medial aspect as compared to lateral aspect.
EPIDEMIOLOGY:
Prevalence is 1 in 1 million
It is three times more common in boys
Non-hereditary of unknown aetiology
First presents between 2-14 years of age
PRESENTATION:
Child usually presents with painless asymmetric firm swelling affecting one side of a lower limb joint.
There may be limb wasting, varus/ valgus deformity, anular deformities, joint locking, limb lengthening discrepancies etc.
Upper limb involvement and bilateral involvement have been described in literature but are extremely rare.
TYPES:
Three types:Localized, classic and generalized
Localized variety: Single bone is affected, usually hindfoot or ankle
Classic variety:Affects more than 1 area in a single lower limb, usually knee and ankle. It accounts for more than two-thirds of the cases
Generalized form: Most severe form. Affects the whole lower limb from pelvis to foot.
IMAGING
Radiography: X-rays reveal mass with early focal ossification in medial or lateral side of the epiphysis (may be one or more). The lesions enlarge and ossify with bone maturation and may unite with the underlying bone. There may be premature closure of epiphysis with resultant limb length discrepancies.
There may be early secondary osteoarthritis .
There may be secondary involvement of metaphysis.
CT: shows anatomic relationship between mass and bone like cortical/ medullary bone continuity
MRI: shows anatomic relations better and also helps in identifying the tumour.
It shows signal intensity of lesion as well as continuity with the primary site.
TREATMENT:
Observation or surgical
Surgery is only indicated if patient presents with severe pain and/ or deformity or if there is locking of the joint.
RECURRENCE: is high after surgery
REFERENCES:
Araujo CR et al:Dysplasia Epiphysealis Hemimelica of Patella.Radiographics. 26:581-6, 2006
Bakarman KA: Dysplasia Epiphysealis Hemimelica.Medscape Radiology