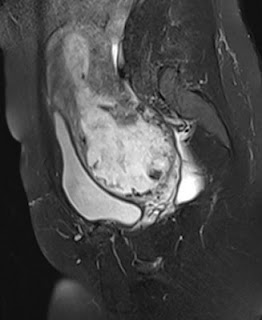
A patient presented in her mid thirties with a first trimester intra-uterine pregnancy having conceived after IVF. USG showed a fetus with cardiac activity and crown-rump length corresponding to 11 weeks' gestation. The gestation sac was abnormally low lying with an empty endometrial cavity above it. The cervix was poorly visualized. An MRI was indicated to rule out true cervical pregnancy.
MRI showed a low lying gestation sac with empty endometrial cavity above it. The cervix was shortened with a closed cervical canal and internal os. There was a large low lying placenta surrounding the sac with loss of interface between the placenta and myometrium. The myometrium was thinned out. A diagnosis of cervico-isthmic pregnancy was made with the likelihood of adherent placenta.
CERVICO-ISTHMIC PREGNANCY
INTRODUCTION: A cervico-isthmic pregnancy is an ectopic pregnancy which implants in the isthmus. The isthmus is the region between the cervix and fundus.
It is a rare complication of pregnancy and is often confused with a cervical pregnancy. Distinguishing between these is crucial as a cervical pregnancy is virtually not viable while there are a few reports of cervico-isthmic pregnancies being carried successfully to term. Also, cervical pregnancies are more dangerous and associated with serious risks like haemorrhage, rupture, blood transfusions, hysterectomy etc.
INCIDENCE:
Incidence of cervical pregnancy: 1:1000 to 1:16000.
Cervico-isthmic pregnancies are more common than true cervical pregnancies.
IMAGING FINDINGS:
USG: Typically, ultrasound shows an empty uterine cavity with a low lying pregnancy. It may be confused with true cervical pregnancy. In a true cervical pregnancy, the sac is completely within the cervix.
MRI: shows a low lying gestation sac with a well preserved and closed cervical canal. It is hence helpful in distinguishing cervical from cervico-isthmic pregnancy.
IMPLICATIONS: Although there are reports of successful cervico-isthmic pregnancies, these pregnacies are also exposed to risks like:
- Spontaneous abortion/ premature delivery
- premature rupture of membranes
- placenta accreta
- postpartum hemorrhage
- hysterectomy
- Uterine rupture if associated with thinned out myometrium
- Oyelese Y, Elliott T B, Asomani N, Hamm R, Napoli L, Lewis KM: Sonography and Magnetic Resonance Imaging in the Diagnosis of Cervico-Isthmic pregnancy. J Ultrasound Med 2003; 22: 981-983
- Strobelt N, Locatelli A, Ratti M, Ghidini A: Cervico-isthmic pregnancy: a case report, critical appraisal of the diagnostic criteria, and reassessment of the outcome. Acta Obstet Gynecol Scand 2001; 80: 586-588.
- Jelsema RD, Zuidema L: First trimester diagnosed cervico-isthmic pregnancy resulting in term delivery. Obstet Gynecol 1992; 80: 517-519
- Wikipedia